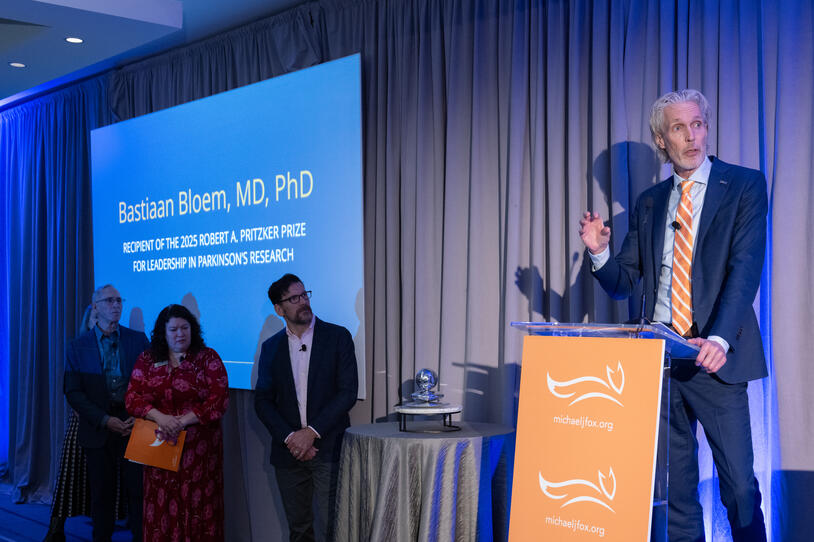
Bastiaan (Bas) Bloem, MD, PhD, accepting the 2025 Robert A. Pritzker Prize for Leadership in Parkinson's Research.
Bastiaan (Bas) Bloem, MD, PhD, is helping redefine what it means to care for people with Parkinson’s disease. Recently honored with the 2025 Robert A. Pritzker Prize for Leadership in Parkinson’s Research by The Michael J. Fox Foundation for Parkinson’s Research (MJFF), Dr. Bloem was recognized not only for groundbreaking science but for championing a holistic, person-first approach that addresses the condition from many angles.
As a professor of movement disorder neurology and director of the Center of Expertise for Parkinson’s Disease at Radboud University Medical Center in the Netherlands, Dr. Bloem has spent decades proving that Parkinson’s treatment goes beyond medication. His research underscores the power of lifestyle interventions — exercise, stress management, social connection and more — as essential tools for improving quality of life and potentially slowing disease progression.
“When I face people with Parkinson’s in my clinic, the ones doing the best are the ones who adhere to a healthy lifestyle,” he said.
Here, Dr. Bloem shares five lifestyle strategies that can help people with Parkinson’s live well today — and possibly change the future of their disease.
Movement Matters as Much as Medicine
A former player on the Dutch national volleyball team, Dr. Bloem understood the power of physical exercise well before he became a doctor. Now, research by Dr. Bloem and others confirms what he has long believed: exercise plays a critical role in managing Parkinson’s. Its benefits reach far past fitness — improving sleep, mobility and balance while easing depression and constipation.
“It helps alleviate motor symptoms, but also non-motor symptoms,” he said. “It works like a drug, which means if you stop, you lose the benefits.”
Dr. Bloem emphasized that exercise cannot replace today’s transformative medications. However, it is a vital complement, strengthening both the body and brain. “People often think, ‘Oh, is the goal of lifestyle interventions to reduce medication?’ No, you need to be in a good ‘on’ phase to get a good workout. You need both,” he added.
Exercise Could Be a Disease-modifying Therapy
While many questions remain, Dr. Bloem’s own studies add weight to growing evidence that non-pharmacological approaches — such as exercise — may slow or even stop Parkinson’s progression.
His Park-in-Shape trial demonstrated that home-based workouts sparked new connections between the damaged basal ganglia and the healthy cortex, meaning that the healthy areas of the brain start to take over the functions of the areas damaged due to Parkinson’s. Building on that information, his ongoing Slow-SPEED study, partially funded by MJFF, is exploring whether exercise at the earliest stages of Parkinson’s could delay or prevent future symptoms.
“Exercise might be the world’s very first disease-modifying intervention,” he said.
Build a Routine with “Exercise Snacks”
Maintaining a consistent exercise routine is often difficult, particularly for those living with chronic conditions like Parkinson’s disease, where physical and cognitive challenges create additional barriers.
Dr. Bloem advises aiming for 30 minutes of exercise at least three times a week — ideally, every day. While that goal can feel overwhelming for some, emerging research suggests that brief bursts of movement may be as effective as longer workouts.
His practical solution? What he calls “exercise snacks.” Instead of carving out a full half-hour, break the activity into bite-sized segments. For example, climbing stairs for just two minutes might seem minor, but you’ll hit your target if you repeat that 15 times throughout the day.
The Importance of Stress Management
Many people with Parkinson's disease experience chronic stress, which can bring on or worsen their symptoms.
Mindfulness, or meditation — incorporating breathing exercises and relaxation techniques — can ease stress and lift mood. Dr. Bloem suspects it might do even more: his team is studying brain scans before and after mindfulness training to explore whether these practices can change the course of Parkinson’s disease.
“We know from animal studies that chronic stress may harm dopamine-producing neurons and hasten disease progression,” he explained. “If you reduce stress, you could slow down that progression.”
Connecting with Others Is Key
Parkinson’s can feel isolating — and that’s why staying connected matters as much as staying active. Dr. Bloem stresses that pairing exercise with social interaction amplifies its benefits, improving not only physical health but emotional well-being. Across the country, group classes designed for people with Parkinson’s, such as boxing, dance, yoga and tai chi offer a chance to move, laugh and belong.
“What makes us human is connection,” said Dr. Bloem. “Anything that brings people together is essential.”