COVID has been in the news for over two years now. But the potential connection between COVID and Parkinson’s is back in the headlines. This time, it’s based on recent research led by Richard Smeyne, PhD, of Thomas Jefferson University in Philadelphia, Pennsylvania and published in the journal Movement Disorders. The study, conducted in pre-clinical models, suggests that COVID could play a role in bringing on Parkinson’s disease (PD).
To learn more, we spoke with James Goldman, MD, PhD, a neuropathologist who studies brain tissue to learn about and diagnose disease, at Columbia University in New York, New York.
The Michael J. Fox Foundation (MJFF): Let’s start with the question on many minds. Does COVID cause Parkinson’s?
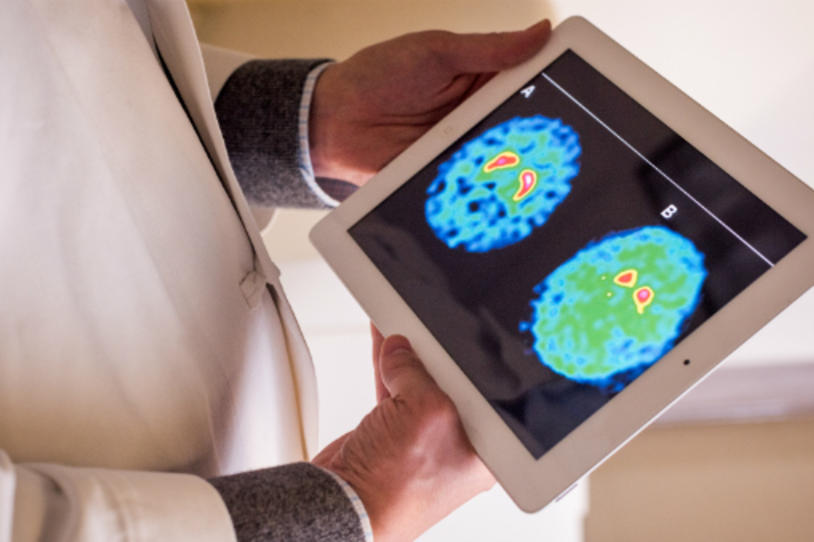
James Goldman (JG): There’s no easy answer to that question. I can tell you that as a neuropathologist, I have looked at a large number of brains of people who’ve died of COVID. In the substantia nigra, the brain area that’s affected by Parkinson’s, there’s very little to see. There is no evidence of nerve cell degeneration. There is, however, a lot of change in other areas of the brain. There is damage from hypoxia (low oxygen) that likely results from pulmonary (lung) problems with COVID. There are also, in some people, small infarcts (strokes). And there is activation of microglial cells, the brain’s immune cells. This is a sign of inflammation, which can cause damage to brain cell function. So there is a great deal of pathology that occurs in the brains of people who die from COVID, but nothing we can directly relate to the known pathology of Parkinson’s.
We and others also have found rather little evidence for virus in the brain itself. So, the changes we see in the brain are not likely due to a direct effect of virus in the brain.
One caveat is that our findings are based on what we see in patients who die from COVID infection, and therefore have the most severe illness. While we think that some of these changes also occur in the brains of people who survive COVID, we don’t know for sure. We have looked at the brains of people who survived acute COVID infection but died months later from something else (cancer or heart disease, for example), and we see many of the same changes. But we don’t know if these came on during the COVID infection and remained or if, instead, the changes resulted from the illness that caused the individual’s death.
MJFF: Tell us about the recent research on COVID and Parkinson’s in the news.
JG: The first comment I have is about research on these types of pre-clinical models of Parkinson’s. In general, it’s not clear how good these are at mimicking human brain pathology. Meaning, if you see something in a pre-clinical model, you may or may not see the same in a human brain. The results of this and similar papers seem to be a bit at odds with what we see at autopsy of human brains. For example, we don’t see COVID virus in the brain, but researchers often see it in these models.
As for this study, what the researchers find is interesting. If they give COVID virus or a small dose of MPTP (a toxin that destroys dopamine nerve cells) to pre-clinical models, there isn’t much change in the substantia nigra, the brain area impacted by Parkinson’s. But if they give both COVID and MPTP, they see loss of dopamine nerve cells in the substantia nigra as well as activation of microglial cells. This suggests that the virus somehow sensitizes nerve cells to the stress of the MPTP toxin. It’s important to note that a) they aren’t giving mice the equivalent of human Parkinson’s disease, just showing nerve cell death and b) this may not be unique to COVID as similar findings have been seen with influenza (the flu) in these models.
I would not say this paper proves that COVID causes Parkinson’s disease. I think that’s a big stretch.
MJFF: Could inflammation (as shown by microglial activation) trigger Parkinson’s?
JG: No one knows the answer to that. Could a viral disease — COVID, influenza or something else — that produces hypoxia or systemic inflammation affect the brain in a way that somehow sensitizes it to potential problems months or years later? We don’t yet know, but it’s an interesting and important question.
MJFF: What about the few cases of Parkinson’s reported after a COVID infection?
JG: My sense is that there was something already going on in the brains of these individuals, before the COVID infection. Meaning, Parkinson’s or parkinsonism (symptoms of Parkinson’s) were not yet detectable, but brain changes were happening. Whether or not the COVID infection damaged brain cells or impacted brain pathways really isn’t clear, although the hypoxia and inflammation that individuals with COVID experience could have theoretically produced enough change to tip the brain over a threshold that produced visible symptoms of Parkinson’s.
MJFF: What about smell loss and COVID?
JG: At autopsy of people who died from COVID, we’ve seen very clearly that the virus (and other changes) are present in the olfactory epithelium, the nasal cavity membrane that supports smell. This is not unexpected and could explain smell loss (anosmia). We have not seen, however, evidence of virus in the olfactory epithelium nerve cells, which transmit sense of smell to the brain. So, it doesn’t seem there is evidence that virus gets taken up by nerve cells and transported along to the brain in this manner. Nevertheless, colleagues of mine at Columbia have found that the olfactory nerve cells in people with COVID do lose their sensitivity to odors, which likely causes anosmia.
MJFF: What are next steps to figuring out if COVID causes Parkinson’s?
JG: As a neuropathologist, I think continued study of the brains of people who pass away after surviving COVID and later developing Parkinson’s, especially if they are younger than the average age of Parkinson’s onset, will help.
MJFF: If I had COVID, should I worry about getting Parkinson’s?
JG: If you weren’t worried about Parkinson’s before, I’d say don’t start because of COVID. I think it’s too early to see what’s going to happen. My outlook in general is that losing sleep over something like this isn’t useful. Try instead to channel your energy into leading a healthy lifestyle, with regular exercise, a healthy diet and other positive activities.
